A man stumbled on level ground, unsuccessfully opened a heavy door, or dropped a weighty book on his leg. It would seem a trifle. And for a patient with osteoporosis, the case may end in a fracture.
Definition
The name of this disease comes from two Greek words: osteon – bone and poros – hole. Thus, osteoporosis is a special disease that affects bone tissue, in which voids-pores are formed in it. From this, the bones of our skeleton become extremely fragile and can break even under light loads.
Symptoms
Usually this condition does not manifest itself in the early stages. But as the bone tissue weakens, the following symptoms may appear:
back pain caused by destruction of the vertebra;
decrease in growth over time;
slouch;
a bone fracture that occurs with a slight load.
Your doctor should be consulted if:
menopause has begun;
corticosteroid therapy was carried out for several months;
a hip fracture occurred in old age.
Causes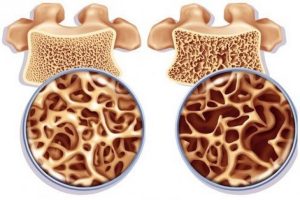
Bone tissue is in a state of continuous renewal: old tissue is absorbed and new tissue is created. In adolescence, new bone tissue is created faster, so its mass grows. Most people reach their peak bone mass before age 20. In old age, bone tissue is absorbed faster than it is restored. The tendency to osteoporosis also depends in part on the bone mass achieved in adolescence. The more bone mass is achieved in the peak period, the more bone tissue is in the “reserve”, and the less the tendency to develop osteoporosis in old age.
Risk factors
The propensity to develop the disease depends on many factors: age, race, lifestyle, medications taken.
Uncontrollable factors
Some risk factors are difficult to control, for example:
Floor. Women are more prone to developing the disease.
Age. The older the age, the higher the risk.
Race. Persons of Asian or Caucasian origin are at greatest risk.
Family history. The greatest risk in the presence of osteoporosis is in direct relatives, especially in the case of a hip fracture in one of the parents.
Skeleton dimensions. People with low bone mass are at greatest risk.
Hormone levels
Most often, osteoporosis is found in patients with an excess or deficiency of certain hormones in the body. These factors are:
Sex hormones. Decreased levels of sex hormones reduce bone strength. A decrease in estrogen concentration in postmenopausal women is one of the most influential risk factors for osteoporosis. In men, testosterone levels gradually decrease with age. Prostate cancer treatments that suppress testosterone production and breast cancer treatments that decrease estrogen levels accelerate bone loss.
Thyroid disorders. Excess thyroid hormone contributes to the weakening of the bone. This can happen with an overactive gland or with treatment with thyroid hormones.
Disorders of other endocrine glands. Osteoporosis is also associated with overactive parathyroid and adrenal glands.
Nutritional factors
Osteoporosis most often occurs in patients with the following abnormalities:
Insufficient calcium intake. Calcium deficiency plays a large role in the development of osteoporosis. A low intake of calcium in the body leads to a decrease in bone density, early bone loss and an increased risk of fractures.
Digestive disorders. Severely reducing food intake and being underweight weakens bones in both men and women.
Operations on the digestive organs. Surgery to reduce the volume of the stomach or to remove part of the small intestine limits the absorption of nutrients, including calcium.
Steroids and other medications
Long-term use of oral or injectable corticosteroids such as prednisone and cortisone interferes with bone repair. Osteoporosis is also associated with drugs for treatment or prevention:
– gastric reflux (heartburn);
– transplant rejection;
– seizures;
– cancer.
Various diseases The risk of osteoporosis is higher in patients with the following disorders: – celiac disease; – inflammatory bowel lesions; – kidney or liver disease; – lupus; – multiple myeloma; – rheumatoid arthritis.
Lifestyle
Certain bad habits can increase your risk of developing osteoporosis, for example:
Passive lifestyle. People who spend a lot of time sitting are at higher risk of developing osteoporosis than those who are active. Any kind of activity is helpful, especially walking, running, jumping, dancing, and lifting weights.
Alcohol abuse. Regular consumption of more than two drinks per day increases the risk of developing the disease.
Tobacco smoking. There is currently no clear understanding of the role of tobacco in osteoporosis, but smoking has been shown to reduce bone strength.
Complications
Fractures of the bones, especially the vertebrae or the femur, are the most serious complications of osteoporosis. Femur fractures are common in a fall and can lead to disability and an increased risk of death within the first year after injury. In some cases, vertebral fractures occur even without falling. The vertebrae that make up the spine can weaken to the point that they begin to crumple, leading to back pain, decreased height, and stoop.
Diagnostics
Bone density can be measured with an apparatus that uses low-intensity X-rays to determine bone mineralization. In this painless examination, the patient is scanned in a supine position. In most cases, the density of only some bones is measured, usually the femur, spine, and wrist bones.
Treatment
Treatment recommendations are often based on an assessment of the risk of a bone fracture in the next 10 years using bone density measurements. If this risk is low, therapy may be drug-free and focus on modifying risk factors that weaken bone.
For both men and women at increased risk of fracture, bisphosphonates are most commonly prescribed, which include: – alendronate; – risedronate; – ibandronate; – zoledronic acid.
Side effects include nausea, abdominal pain, and heartburn. Intravenous bisphosphonates do not cause stomach upset but can cause fever, headache, and muscle pain within 3 days. Bisphosphonates are also capable of affecting the mandible. Osteoporosis of the lower jaw is a rare condition that usually occurs after tooth extraction, when the tooth socket does not overgrow. Therefore, you should have a dental check-up before you start taking bisphosphonates.
Hormone therapy
Estrogens, especially taken soon after menopause, can help normalize bone density. However, estrogen therapy can increase the risk of blood clots, endometrial cancer, breast cancer, and heart disease. Thus, estrogens are commonly used to maintain bone health in young women or in menopausal women. Raloxifene has estrogen-like effects on bone in postmenopausal women, but without some of the estrogenic health risks. Taking this drug may reduce the risk of certain types of breast cancer. The most common side effect is hot flashes. The risk of blood clots may also be increased. In men, osteoporosis may be associated with a gradual decline in testosterone concentrations. Testosterone replacement therapy can help combat symptoms of hormone deficiency, but for osteoporosis, it is better to use special therapy or combine it with hormonal therapy.
Alternative therapy
Soy protein https://en.wikipedia.org/wiki/Soy_protein has a similar effect to estrogen on bone tissue. Some studies indicate that the risk of bone fracture is reduced among menopausal Asian women who consume large amounts of soy protein. But it should be consumed with caution in women with a family history of breast cancer. Most soy foods have not been shown to affect the risk of bone fracture.
